Pathophysiology[edit]
Main article: Carcinogenesis
Breast cancer, like other cancers, occurs because of an interaction between an environmental (external) factor and a genetically susceptible host. Normal cells divide as many times as needed and stop. They attach to other cells and stay in place in tissues. Cells become cancerous when they lose their ability to stop dividing, to attach to other cells, to stay where they belong, and to die at the proper time.
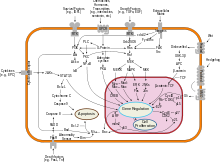
Normal cells will commit cell suicide (apoptosis) when they are no longer needed. Until then, they are protected from cell suicide by several protein clusters and pathways. One of the protective pathways is the PI3K/AKT pathway; another is the RAS/MEK/ERK pathway. Sometimes the genes along these protective pathways are mutated in a way that turns them permanently "on", rendering the cell incapable of committing suicide when it is no longer needed. This is one of the steps that causes cancer in combination with other mutations. Normally, the PTEN protein turns off the PI3K/AKT pathway when the cell is ready for cell suicide. In some breast cancers, the gene for the PTEN protein is mutated, so the PI3K/AKT pathway is stuck in the "on" position, and the cancer cell does not commit suicide.[63]
Mutations that can lead to breast cancer have been experimentally linked to estrogen exposure.[64]
Abnormal growth factor signaling in the interaction between stromal cells and epithelial cells can facilitate malignant cell growth.[65][66] In breast adipose tissue, overexpression of leptin leads to increased cell proliferation and cancer.[67]
In the United States, 10 to 20 percent of patients with breast cancer and patients with ovarian cancer have a first- or second-degree relative with one of these diseases. The familial tendency to develop these cancers is called hereditary breast–ovarian cancer syndrome. The best known of these, the BRCA mutations, confer a lifetime risk of breast cancer of between 60 and 85 percent and a lifetime risk of ovarian cancer of between 15 and 40 percent. Some mutations associated with cancer, such as p53, BRCA1 andBRCA2, occur in mechanisms to correct errors in DNA. These mutations are either inherited or acquired after birth. Presumably, they allow further mutations, which allow uncontrolled division, lack of attachment, and metastasis to distant organs.[48][68] However, there is strong evidence of residual risk variation that goes well beyond hereditaryBRCA gene mutations between carrier families. This is caused by unobserved risk factors.[69] This implicates environmental and other causes as triggers for breast cancers. The inherited mutation in BRCA1 or BRCA2 genes can interfere with repair of DNA cross links and DNA double strand breaks (known functions of the encoded protein).[70] These carcinogens cause DNA damage such as DNA cross links and double strand breaks that often require repairs by pathways containing BRCA1 and BRCA2.[71][72] However, mutations in BRCA genes account for only 2 to 3 percent of all breast cancers.[73] Levin et al. say that cancer may not be inevitable for all carriers of BRCA1 and BRCA2mutations.[74] About half of hereditary breast–ovarian cancer syndromes involve unknown genes.
GATA-3 directly controls the expression of estrogen receptor (ER) and other genes associated with epithelial differentiation, and the loss of GATA-3 leads to loss of differentiation and poor prognosis due to cancer cell invasion and metastasis.[75]
No comments:
Post a Comment