Diagnosis[edit]
Performing a chest radiograph is one of the first investigative steps if a person reports symptoms that may suggest lung cancer. This may reveal an obvious mass, widening of the mediastinum (suggestive of spread to lymph nodes there), atelectasis (collapse), consolidation (pneumonia) or pleural effusion.[2] CT imaging is typically used to provide more information about the type and extent of disease.Bronchoscopy or CT-guided biopsy is often used to sample the tumor for histopathology.[14]
Lung cancer often appears as a solitary pulmonary nodule on a chest radiograph. However, the differential diagnosis is wide. Many other diseases can also give this appearance, including tuberculosis, fungal infections, metastatic cancer or organizing pneumonia. Less common causes of a solitary pulmonary nodule include hamartomas, bronchogenic cysts, adenomas, arteriovenous malformation,pulmonary sequestration, rheumatoid nodules, granulomatosis with polyangiitis, or lymphoma.[55] Lung cancer can also be an incidental finding, as a solitary pulmonary nodule on a chest radiograph or CT scan done for an unrelated reason.[56] The definitive diagnosis of lung cancer is based on histological examination of the suspicious tissue in the context of the clinical and radiological features.[1]
Clinical practice guidelines recommend frequencies for pulmonary nodule surveillance.[57] CT imaging should not be used for longer or more frequently than indicated as extended surveillance exposes people to increased radiation.[57]
Classification[edit]
| Histological type | Incidence per 100,000 per year |
|---|---|
| All types | 66.9 |
| Adenocarcinoma | 22.1 |
| Squamous-cell carcinoma | 14.4 |
| Small-cell carcinoma | 9.8 |
Lung cancers are classified according to histological type.[8] This classification is important for determining management and predicting outcomes of the disease. Lung cancers are carcinomas—malignancies that arise from epithelial cells. Lung carcinomas are categorized by the size and appearance of the malignant cells seen by a histopathologist under a microscope. For therapeutic purposes, two broad classes are distinguished: non-small-cell lung carcinoma and small-cell lung carcinoma.[58]
Non-small-cell lung carcinoma[edit]
The three main subtypes of NSCLC are adenocarcinoma, squamous-cell carcinoma andlarge-cell carcinoma.[1]
Nearly 40% of lung cancers are adenocarcinoma, which usually originates in peripheral lung tissue.[8] Although most cases of adenocarcinoma are associated with smoking, adenocarcinoma is also the most common form of lung cancer among people who have smoked fewer than 100 cigarettes in their lifetimes ("never-smokers").[1][59] A subtype of adenocarcinoma, the bronchioloalveolar carcinoma, is more common in female never-smokers, and may have a better long-term survival.[60]
Squamous-cell carcinoma accounts for about 30% of lung cancers. They typically occur close to large airways. A hollow cavity and associated cell death are commonly found at the centre of the tumour.[8] About 9% of lung cancers are large-cell carcinoma. These are so named because the cancer cells are large, with excess cytoplasm, large nuclei and conspicuous nucleoli.[8]
Small-cell lung carcinoma[edit]
In small-cell lung carcinoma (SCLC), the cells contain dense neurosecretory granules (vesicles containing neuroendocrine hormones), which give this tumor an endocrine/paraneoplastic syndrome association.[61] Most cases arise in the larger airways (primary and secondary bronchi).[14] These cancers grow quickly and spread early in the course of the disease. Sixty to seventy percent havemetastatic disease at presentation. This type of lung cancer is strongly associated with smoking.[1]
Others[edit]
Four main histological subtypes are recognised, although some cancers may contain a combination of different subtypes.[58] Rare subtypes include glandular tumors, carcinoid tumors, and undifferentiated carcinomas.[1]
Metastasis[edit]
| Histological type | Immunostain |
|---|---|
| Squamous-cell carcinoma | CK5/6 positive CK7 negative |
| Adenocarcinoma | CK7 positive TTF-1 positive |
| Large-cell carcinoma | TTF-1 negative |
| Small-cell carcinoma | TTF-1 positive CD56 positive Chromograninpositive Synaptophysinpositive |
The lung is a common place for the spread of tumours from other parts of the body. Secondary cancers are classified by the site of origin; e.g., breast cancer that has spread to the lung is called metastatic breast cancer. Metastases often have a characteristic round appearance on chest radiograph.[62]
Primary lung cancers themselves most commonly metastasize to the brain, bones, liver and adrenal glands.[8] Immunostaining of a biopsy is often helpful to determine the original source.[63]
Staging[edit]
See also: Lung cancer staging
Lung cancer staging is an assessment of the degree of spread of the cancer from its original source. It is one of the factors affecting the prognosis and potential treatment of lung cancer.[1]
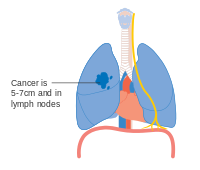
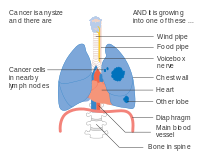
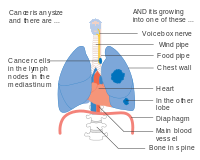
The initial evaluation of non-small-cell lung carcinoma (NSCLC) staging uses the TNM classification. This is based on the size of the primary tumor, lymph node involvement, and distant metastasis.[1]
|
|
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Using the TNM descriptors, a group is assigned, ranging from occult cancer, through stages 0, IA (one-A), IB, IIA, IIB, IIIA, IIIB and IV (four). This stage group assists with the choice of treatment and estimation of prognosis.[65]
| TNM | Stage group |
|---|---|
| T1a–T1b N0 M0 | IA |
| T2a N0 M0 | IB |
| T1a–T2a N1 M0 | IIA |
| T2b N0 M0 | |
| T2b N1 M0 | IIB |
| T3 N0 M0 | |
| T1a–T3 N2 M0 | IIIA |
| T3 N1 M0 | |
| T4 N0–N1 M0 | |
| N3 M0 | IIIB |
| T4 N2 M0 | |
| M1 | IV |
Small-cell lung carcinoma (SCLC) has traditionally been classified as "limited stage" (confined to one half of the chest and within the scope of a single tolerable radiotherapy field) or "extensive stage" (more widespread disease).[1] However, the TNM classification and grouping are useful in estimating prognosis.[65]
For both NSCLC and SCLC, the two general types of staging evaluations are clinical staging and surgical staging. Clinical staging is performed prior to definitive surgery. It is based on the results of imaging studies (such as CT scans and PET scans) and biopsy results. Surgical staging is evaluated either during or after the operation, and is based on the combined results of surgical and clinical findings, including surgical sampling of thoracic lymph nodes.[8]
- Diagrams of main features of staging










No comments:
Post a Comment